Many healthcare organizations depend on exchanging electronic enrollment information with business partners for administering health benefits and processing insurance claims. This standard transaction provides a standardized format for this essential data exchange between healthcare entities. However, successfully implementing the EDI 834 process to maintain accurate member enrollment information involves navigating a complex multi-step process. Many organizations struggle to understand the end-to-end EDI services along with the best practices needed to maximize their value. This blog aims to provide a clear and simple step-by-step guide to the EDI 834 process from start to finish.
Overview of the EDI 834 process
The process of EDI 834 refers to the steps involved in electronically exchanging member enrollment data using HIPAA 834 transactions. At a high level, the process typically involves the following:
- The sender first collects enrollment information from sources which includes member demographics and coverage details. This data provides the information required to create the standardized transactions.
- Next, the sender creates files from the collected enrollment data in the required HIPAA format. The 834 file contains member enrollment records in the standard layout defined by the ASC X12N 834 Implementation Guide.
- The sender then performs validation checks on the Edi files to ensure accuracy, completeness, and compliance with HIPAA requirements. Any errors are corrected before finalizing the files for transmission.
- The validated 834 files are then transmitted to the intended receiver via secure channels like FTP or EDI 834 process. The receiver acknowledges successful reception and communicates any errors back to the sender.
- The receiver then processes the received EDI 834 files by extracting member records, mapping data to their internal fields, translating them to the native format, and loading them into their enrollment systems.
- Regular reconciliation and auditing are performed by trading partners to identify and resolve any mismatches in membership data, ensuring end-to-end data accuracy throughout the EDI 834 process.
Eliminate Manual Data Entry with EDI
Importance of understanding the EDI 834 process
Healthcare organizations rely on accurate and up-to-date member enrollment data to effectively administer health insurance benefits, process claims, coordinate care, and report on key metrics. The process plays a crucial role in facilitating the secure and standardized electronic exchange of this important data between organizations. Therefore, understanding how the EDI 834 process works end-to-end and implementing it properly is critical for several reasons:
- Data Accuracy –Only by thoroughly knowing each step in the EDI 834 process can an organization ensure complete and error-free enrollment data is collected, formatted, transmitted, and updated via healthcare EDI transactions. Inaccurate or incomplete data can impact crucial functions like claims payments, eligibility verifications, and risk scoring.
- Compliance – Strict compliance with HIPAA 834 guidelines is required to avoid penalties and enforceable actions. A comprehensive knowledge of the 834 EDI process helps identify and address any areas of non-compliance that need remediation.
- Cost Savings– Electronic data exchange via 834 transactions provides significant cost reductions compared to manual methods. However, fully realizing these savings relies on correctly executing each step in the 834 processes from beginning to end.
- Customer Service- Timely and accurate member eligibility information received via 834 transactions. It helps top EDI providers deliver better care coordination and a positive patient experience, which can positively impact customer satisfaction scores.
- Improvements – Knowing in detail how the current 834 process operates helps identify areas for optimization and innovation.
Benefits of using the EDI 834 process in the healthcare industry
Electronic data interchange (EDI) allows healthcare organizations to securely and efficiently exchange important administrative and clinical data in a standardized format. The use of the EDI 834 process, including HIPAA-compliant EDI transactions offers several key benefits to the healthcare industry:
- Data Accuracy – The EDI process reduces errors by using consistent data definitions and standardized formats for healthcare EDI transactions. This leads to more accurate data sharing between organizations.
- Faster Transactions – The EDI 834 process enables the automatic electronic exchange of data as soon as it becomes available, speeding up important processes that rely on information sharing. This leads to time savings.
- Lower Costs – EDI 834 process transactions cost less than manual methods like phone, fax, or mail since they require less human intervention and effort. This improves efficiency and reduces operating expenses.
- Higher Efficiency – The process streamlines processes by automating repetitive tasks, eliminating redundant data entry, and minimizing manual reconciliation between organizations. This improves productivity and throughput.
- Interoperability – The process uses standardized formats defined by HIPAA and X12 to facilitate the interoperable exchange of data between disparate healthcare systems. This eases information sharing across the industry.
- Compliance – Healthcare organizations rely on the process to comply with HIPAA requirements for electronic transactions and code sets. Other process methods make compliance difficult.
- Better Patient Care – The 834 EDI process facilitates faster, easier, and more accurate sharing of patient information between EDI solution providers in the USA. This supports care coordination, utilization management, disease monitoring, and other processes that improve patient outcomes.
The use of standardized EDI 834 transactions offers numerous benefits like reduced costs, improved accuracy, higher security, and interoperability that help the U.S. healthcare system become more efficient, effective, and responsive to the needs of patients.
Purpose and significance of the EDI 834 process
The EDI 834 process serves an important purpose in the healthcare system by facilitating the electronic exchange of member enrollment data. The 834 transaction standardizes the format used to transmit critical information about health plan enrollees between entities.
The main purpose of the EDI 834 process is to enable the accurate and timely transfer of enrollment data in a secure, interoperable, and HIPAA-compliant manner. This allows health plans, providers, employers, and government agencies to optimize key administrative processes that rely on up-to-date member eligibility information.
The 834 EDI process plays an important role by acting as an interoperability layer that supports the flow of standardized enrollment details between different organizations. This enables seamless information exchange that is crucial to the overall functioning of the U.S. healthcare system.
Key stakeholders involved in the EDI 834 process
Several key stakeholders are involved in exchanging member enrollment data using EDI 834 process transactions.
- Health plans use 834 transactions to receive eligibility updates from employers, providers, and government programs. Accurate data helps with claims processing, risk adjustment, and reporting.
- Employers send 834 transactions to health plans to ensure correct premium billing and deductions for employees. They also use 834 data to analyze healthcare spending.
- Providers rely on 834 information from health plans and patients to verify eligibility and coverage before rendering services. This helps minimize claim denials and delays.
- Government programs like Medicare and Medicaid exchange 834 data with health plans and employers to facilitate proper beneficiary enrollment and reimbursement.
- EDI solution providers act as intermediaries by processing 834 transactions between entities that lack direct connectivity. They ensure compliance with HIPAA standards.
- Pharmacy benefit managers use 834 transactions to maintain correct membership rosters for administering prescription drug benefits.
Tired of Manual Data Entry Delays? EDI 834 Makes It Easy
Steps involved in the EDI 834 processes
Gathering Enrollment Data
The first step in the 834 EDI process is for the sender to accurately gather all required member enrollment data. This data provides the required information to create healthcare EDI transactions. The sender can collect enrollment data from a variety of EDI solutions for small businesses including:
- Employee enrollment forms and applications
- HR and benefits management systems
- Health plan and insurance carrier portals
- Government program eligibility records
- Pharmacy benefit manager systems
The collected enrollment data must include all necessary member information defined in the HIPAA 834 Implementation Guide. This includes:
- •Member demographics like name, DOB, gender, and address
- •Member and dependent identifier numbers
- •Coverage selections and effective dates
- Subscriber and policy information
- •Claims administration details
- •Any remarks related to member eligibility
The entity generating the 834 transaction needs to have reliable resources and processes in place to consistently gather complete and accurate enrollment data for all members. Incomplete or incorrect data can compromise the whole EDI process.
Creating the EDI Process File
After accurately gathering all required member enrollment data, the next step is to create the actual EDI 834 file for transmission. The sender uses either a proprietary or third-party EDI 834 solution to format the collected enrollment data into the standardized HIPAA 834 transaction layout.
The EDI 834 file contains identifying data for both the sender and receiver, along with a document control number for traceability. Each member’s data is stored in a separate repeated segment within the file with required fields populated based on the enrollment information collected.
The specific EDI 834 format used – either flat file with delimiters or XML with tags – depends on the requirements and capabilities of the trading partners. Before transmitting the EDI 834 file, the sender needs to validate the file to ensure:
- It contains data for all required fields
- Field sizes and data types match HIPAA standards
- Values fall within accepted code ranges
- Required checks like name & ID number matches are done
Any errors identified during validation need to be corrected before the 834 files are finalized for transmission.
Thoroughly checking the EDI 834 file for accuracy, completeness, and compliance is crucial as errors can severely impact the enrollment update process.
Mapping and Translation
Mapping and translation are important steps in the EDI 834 process that allow trading partners to properly interpret each other’s 834 transactions. It refers to creating a crosswalk between the sender’s internal data elements or fields and the corresponding elements in the HIPAA standard. This ensures the sender provides data in the exact format required by the healthcare EDI transactions.
Translation refers to converting data between different EDI 834 formats. For example, translating the sender’s native format into the standard 834 formats that the receiver can understand. Trading partners often need to map their internal systems and translate data before exchanging 834 transactions to ensure interoperability. This is particularly true for:
- Organizations with legacy systems
- Partners with different EDI 834 process capabilities
- Implementations that pre-date HIPAA 834
Mapping tables define the relationship between internal and HIPAA data elements while translation algorithms convert non-standard data into layouts. Both mapping and translation are typically built into EDI 834 gateway or portal EDI service providers before routing EDI healthcare transactions between trading partners.
Want to navigate through the EDI 834 process effortlessly
Get in touch with A3Logics, an expert EDI solution provider
Validating the EDI 834 process file
After creating the EDI 834 file using enrollment data collected, the sender performs a thorough validation of the file before transmission. This ensures the 834 file meets HIPAA standards and will be accepted by the receiver.
Any errors identified during validation are corrected and the validation process is repeated until the 834 file is error-free. Common issues checked for include missing or incomplete data, invalid codes, incorrect field formatting, and mismatching identifiers.
Thorough validation is important because errors in the 834 files can cause issues like a rejection of the whole transaction by the receiver, inaccurate or incomplete member enrollment updates, higher reconciliation efforts, and potential HIPAA non-compliance. Validating the EDI 834 file is a critical checkpoint in the EDI 834 process to ensure accuracy before transmission and avoid issues further down the line.
Testing and Compliance in EDI 834 Process
Comprehensive testing and compliance checks are important parts of the EDI 834 process. Testing helps ensure 834 transactions function as intended before going live with trading partners. It typically involves preparing example 834 files with test data and sending those to test environments for end-to-end testing. Errors identified are corrected and testing is repeated until 834 transactions pass all test cases.
Compliance checks make sure 834 processes and data adhere to all HIPAA and other legal requirements. They often focus on:
- Validating data against HIPAA 834 guidelines
- Ensuring timely transmission of 834 files
- Use secure channels for EDI 834 PROCESS
- Protecting privacy and security of member data
Ongoing monitoring and audits are performed to identify compliance gaps and resolve issues. Corrective and preventive actions are implemented as needed. Both testing and compliance activities require involvement from key stakeholders like IT, information security, legal, and compliance teams.
Regular testing and compliance maintenance are critical to reap the benefits of transitioning to the EDI 834 system. They also help avoid potential fines, breaches, and reputational damage from compliance.
Transmitting the EDI 834 process File
After validating and finalizing the EDI 834 file, the EDI providers proceeded to transmit it to the intended trading partner. Transmission methods for 834transactions include:
- The sender transmits the validated 834 files to the receiver via a secure FTP server, encrypted email, or another agreed-upon secure channel. Some trading partners may also use EDI 834 portals or VANs (value-added networks) to facilitate secure data exchange.
- The receiver downloads the transmitted 834 files and performs initial checks t opportunities prevent malicious attachments.
- Any errors in transmission like incomplete file transfers are quickly identified and resolved.
- After successful reception, the receiver sends the sender an afunctional acknowledgment indicating the 834 files were received and can be processed. This acknowledgment contains none of the member data but only confirms transaction-level details.
- The receiver then disassembles and parses the received 834 files to extract data for their systems. Mapping and translation layers are invoked as needed.
- Any errors in the transmitted data are captured and communicated back to the sender for correction in subsequent 834 files.
Regular transmissions as needed, typically monthly or within events, ensure trading partners have up-to-date sources of membership data for accurate health plan administration.
Error Resolution and Exception Handling
Effective error resolution and exception-handling mechanisms are critical components of the EDI 834 process. They help address any errors or issues identified during the transmission, validation, and processing reconciliation of EDI healthcare transactions.
If the sender identifies errors in an 834 file before transmission, the file is corrected, and the validation process is repeated. Once transmitted, errors are captured in the receiver’s functional acknowledgment and communicated back for correction. The receiver identifies errors during initial validation, data extraction, or loading process. Issues like missing data, format errors, or inconsistent identifiers are reported to the sender promptly.
The sender then makes the necessary corrections to the enrollment data and creates a new and error-free revised 834 file for retransmission. If discrepancies are revealed during reconciliation, both trading partners work to get her to identify the source of issues and determine the correct data. This may require manual research of member records or data from other sources.
A good error resolution process involves:
- Identifying errors as early as possible
- Communicating errors and resolutions between partners
- Correcting root causes in underlying data and processes
- Testing and validating all revisions and EDI 834 process
- Implementing preventive controls to avoid repeat errors
- Documenting all resolution efforts to prove compliance
Adherence to a rigorous error resolution process reduces regulatory risks and helps deliver high-quality, interoperable enrollment data via EDI 834 transactions.
Auditing and Reconciliation
Regular auditing and reconciliation are key parts of the EDI solutions for small businesses to ensure end-to-inaccuracy and compliance. Auditing involves routinely reviewing all aspects by EDI solution providers of the process including:
- Data collection and sources
- Mapping and translation methodologies
- Validation controls and testing
- Transmission and processing procedures
- Error handling and reporting
- Compliance with HIPAA guidelines
Any control gaps, non-compliant practices, or processing issues identified during audits are remediated through corrective and preventive actions. Audits also ensure that member enrollment data exchanged via EDI healthcare transactions remain secure and protected.
Periodic reconciliation involves comparing member information between organizational systems to identify and resolve discrepancies. It typically focuses on member demographics, enrollment status, and coverage details.
Reconciliation helps determine:
- The source and root cause of discrepancies
- Which data source contains the authoritative data
- If corrections are required on either side
- If business rules or policies need to be updated for the future
Trading partners work together during reconciliation to pinpoint data issues, determine correct data values, and agree on a resolution approach. Outstanding differences are resolved before proceeding to the next reconciliation cycle.
Common Challenges of the EDI 834 Process
Like all processes, the EDI 834 process faces common challenges that healthcare organizations need to overcome for successful implementation.
- Initial investment is required to set up the EDI 834 infrastructure including mapping layers, translation engines, secure gateways, and electronic portals to facilitate data exchange.
- Incompatibilities between the internal systems of different trading partners also pose difficulties if their data structures and formats differ significantly. This requires extensive mapping and translation efforts to create interoperability.
Future Trends in the EDI 834 Process
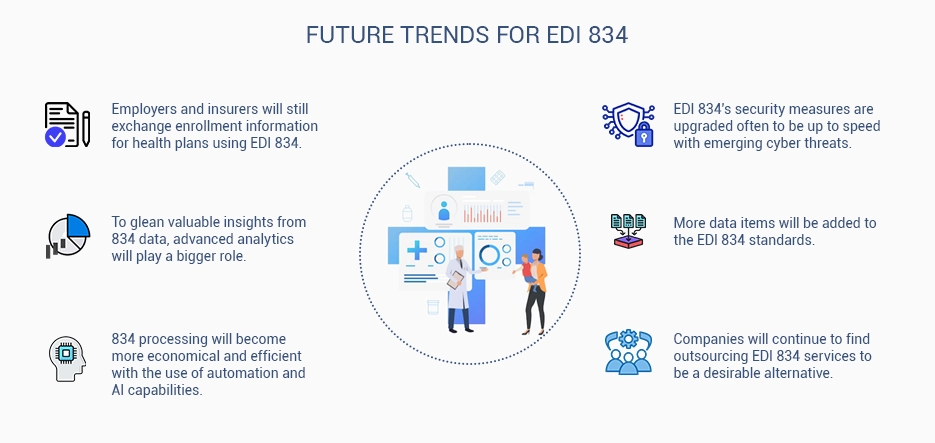
The EDI 834 process is likely to evolve in several ways in the future to keep up with changes in the healthcare industry such as:
- The adoption of the real-time EDI 834 process is expected to increase as organizations move to speed up member enrollment updates and eligibility verifications. This requires investments in new technology and interconnectivity.
- Migration from traditional flat file EDI 834 to XML-based formats is also likely to improve the interoperability, readability, and fault-tolerance of 834 transactions. Utilization of APIs and cloud-based EDI solutions can make the processes easier to implement, scale, and maintain with lower uptime requirements.
Also read: Cloud-Based Healthcare Solutions
Conclusion
The EDI 834 process plays an important role in enabling the electronic exchange of member enrollment data between healthcare organizations. By following the step-by-step guide discussed in this blog, trading partners can effectively implement EDI healthcare transactions to maintain accurate and timely enrollment information.
The key steps involved are:
- properly gathering enrollment data from source systems
- creating standardized files from that data,
- validating the files for accuracy and compliance,
- transmitting the files to the intended receiver and validations by the receiver
- Regular reconciliation, auditing, and error resolution procedures are necessary to ensure the integrity and reliability of the enrollment data exchanged.
While the EDI 834 process faces challenges like high setup costs, data inaccuracies, legacy system limitations, and compliance pressures, there is also an opportunity for investment by emerging trends around the real-time EDI 834 process, API-based solutions, and integration with other health data sources.
Frequently Asked Questions (FAQs)
What is 834 used for?
The EDI 834 transaction is used to electronically exchange member enrollment and benefit plan information between healthcare organizations. It facilitates the accurate, timely, and secure transfer of critical data needed by health plans, EDI vendors , employers, and government programs for important administrative functions like processing insurance claims, administering benefits, verifying eligibility and coverage, performing risk adjustment calculations, reporting and analytics, care coordination, and utilization management, and premium billing and educations. Therefore, the 834 transaction enables healthcare entities to securely share standardized member enrollment details in an electronic, interoperable format that supports the functioning of the entire healthcare ecosystem.
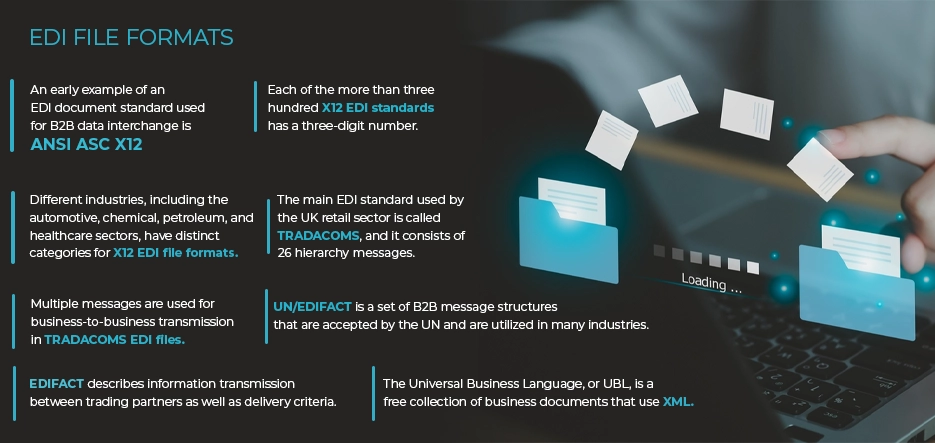
What is x12 834?
The x12 834 transaction, also known as the ASC X12N 834 Benefit Enrollment and Maintenance standard, is an EDI format developed by the Accredited Standards Committee X12 that defines the required data elements and layout for electronically transmitting member enrollment and benefits data. Healthcare organizations use the x12 834 transactions to securely share critical member information ( demographics, coverage selections, & effective dates in a standardized, Interoperable, and HIPAA-compliant manner.
These EDI solutions for small businesses enable electronic data exchange between entities like health plans, providers, employers, and government programs to support important healthcare administrative functions
.
What is the EDI 834 process file feed?
An EDI 834 process file feed refers to the EDI transaction file that is generated and transmitted between trading partners. The EDI 834 process file contains standardized data in a specified form compliant with EDI 834 standards like X12.
EDI 834 file feeds provide critical business data between organizations to streamline processes and maximize efficiency. Common EDI 834 process file feeds include x12 834 benefit enrollment files shared between healthcare entities, x12 810 invoice files between businesses and suppliers, and x12 820 remittance advice files between payers and EDI providers.
What are 834 transactions?
834 transactions refer to electronic data interchange files that contain member enrollment data formatted according to the HIPAA ASC X12N 834 Benefit Enrollment standard. These standardized transactions enable the efficient exchange of enrollment information between entities in the healthcare industry, including health plans, EDI providers, employers, and government programs.
An 834 transaction file typically includes various data elements for each member, such as
- demographic information
- subscriber and dependent identifiers,
- benefit selections, coverage
- eligibility details
- claim administration preference.
Examples of such data elements are names, addresses, dates of birth, gender, member identification numbers, effective dates, contracts, coverage codes, and managed EDI providers assignments.